Arizona Supreme Court’s New Approach to Proving Causation in Emergency Room Malpractice Cases
The recent decision by the Arizona Supreme Court marks a turning point in how emergency room malpractice cases are assessed in the state. The ruling, delivered unanimously, challenges long-held notions regarding expert testimony in cases where negligence is characterized as “likely” the cause of a patient’s injury or death. In doing so, the court opens the door for juries to consider a broader range of evidence, which may ultimately alter the legal landscape for both healthcare providers and plaintiffs in malpractice litigation.
At the heart of the matter lies the case of Henke v. Hospital Development of West Phoenix, Inc., et al. Greg Henke’s tragic experience serves as a stark reminder of the stakes involved when medical professionals make errors in the heat of an emergency. The Arizona Supreme Court’s decision now allows for expert testimony that describes negligence in terms such as “likely” to bear weight in determining causation, a concept that has traditionally been interpreted more rigidly under the “clear and convincing” evidence standard in emergency room malpractice cases.
Understanding the Emergency Room Malpractice Standard: Fine Points of Proving Causation
The Arizona legal system requires plaintiffs in emergency room malpractice cases to satisfy a particularly demanding standard: they must prove causation by clear and convincing evidence. This requirement is meant to ensure that the connection between a healthcare provider’s alleged negligence and the patient’s adverse outcome is both direct and robust. However, establishing this connection has always been one of the trickier parts of medical malpractice litigation.
The new ruling clarifies that the presence of expert testimony stating that negligence “likely” caused an injury should not automatically result in the dismissal of a malpractice claim. Instead, it should prompt a more thorough examination of the evidence available. The decision encourages juries to weigh the “likely” component alongside other available proofs, thereby recognizing that a natural, uninterrupted sequence of events might effectively illustrate a link between alleged negligence and the adverse outcome.
This emphasis on considering the broader picture allows juries to navigate the tangled issues of causation more effectively, ensuring that the jury’s role in considering all evidence is protected under the law.
Legal Journey of Henke v. Hospital Development: Tricky Parts and Obstacles in Medical Malpractice Cases
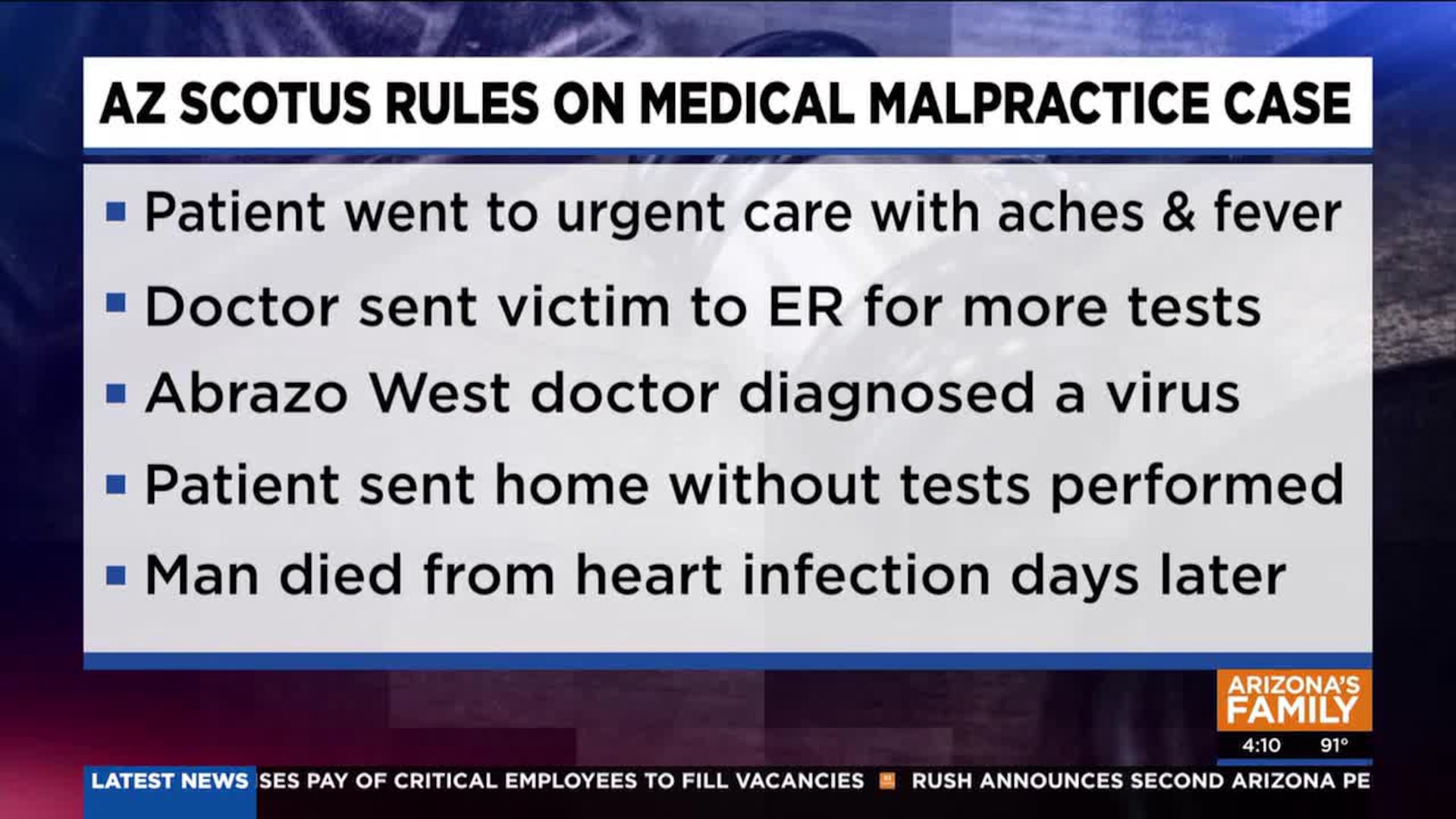
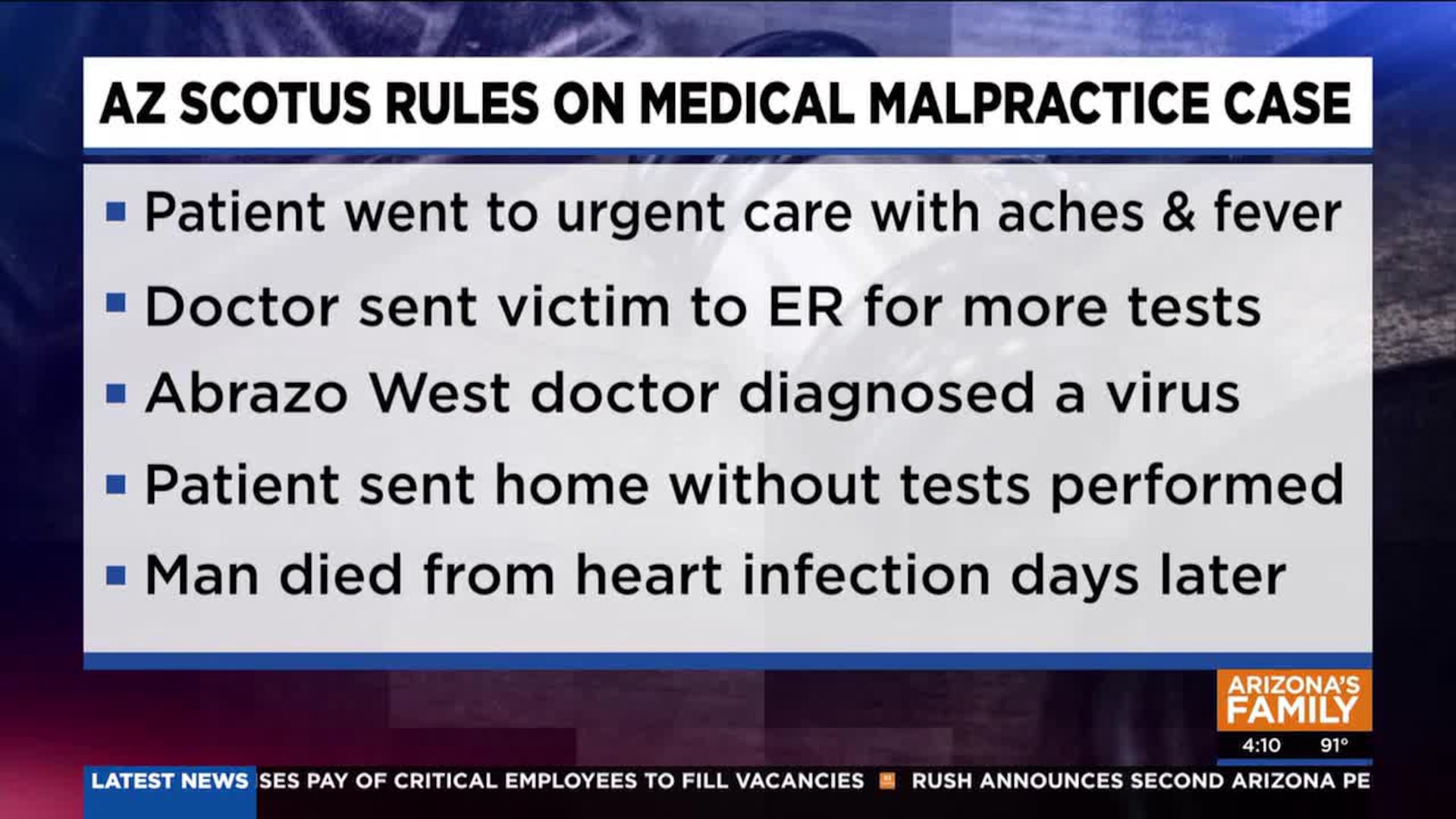
The Henke case provides a clear illustration of how challenging it can be to meet the high bar set by Arizona for proving causation. In March 2017, Greg Henke visited an urgent care facility where he was initially assessed for symptoms that raised alarm bells over a possible bacterial endocarditis infection—a life-threatening condition that affects the heart’s inner lining. Following this preliminary assessment, Henke was directed to the emergency room at Abrazo West Campus.
Greg’s wife, Margarita Henke, recalled that the emergency room staff failed to act on the urgent care doctor’s findings. Instead of pursuing additional tests that could have confirmed bacterial endocarditis, the emergency team dismissed the possibility and instead diagnosed him with a viral condition. Tragically, Greg’s condition deteriorated, and he passed away five days later. An autopsy pointed to complications from sepsis due to acute bacterial endocarditis as the cause of death.
This chain of events not only underscores the critical role that timely and accurate medical intervention plays but also highlights the complicated pieces of evidence collection in such cases. Margarita Henke’s subsequent lawsuit against the hospital claimed that the negligence on the part of the emergency room staff directly led to her husband’s death. Initially, trial judges and even the Court of Appeals sided with the hospital, largely because expert testimony was said to demonstrate only that the negligence “likely” contributed to the death—a phrase that apparently did not equate to the “clear and convincing” standard required by law.
The Arizona Supreme Court’s intervention in this case effectively resets the balance, allowing for a deeper and broader exploration of evidence rather than an outright dismissal based on a potentially narrow view of expert testimony.
Evaluating Expert Testimonies: Getting Into the Debate on “Likely” Causation
One key element of the court’s ruling is the treatment of expert opinions regarding causation. In many malpractice cases, the expert testimony is deemed insufficient if it only suggests that negligence “likely” caused the patient’s adverse outcome. Critics have argued that this language is too vague and can leave significant room for interpretation, which might undermine the standard required under Arizona law.
However, the new opinion emphasizes that the presence of testimony using terms like “likely” should be seen as a starting point rather than conclusive evidence. The court stressed that such testimony is sufficient to establish at least a possible link between the alleged negligence and the resulting harm. This perspective allows the jury to consider a wider array of evidence alongside expert opinions, including:
- Medical records documenting the timeline of treatment
- Eyewitness or staff testimonies regarding the treatment process
- Additional expert opinions that may provide more precise interpretations of the medical evidence
- Statistical data related to treatment outcomes in similar cases
By adopting a more inclusive approach to evidence, the court is essentially empowering the jury to work through the small distinctions and subtle details of the case to arrive at a fair decision. What might have seemed like a nerve-racking or off-putting gap in the evidence is now viewed as a piece of the overall narrative that deserves closer scrutiny.
Implications for Future Emergency Room Malpractice Cases: Sorting Out the Twists and Turns of Legal Evidence
The impact of this decision could be far-reaching. By allowing jury deliberations to incorporate expert testimony that hints at a “likely” connection without dismissing it outright, the Arizona Supreme Court is acknowledging the complexity and the often confusing bits encountered in medical malpractice litigation.
Some potential implications include:
- Broader Jury Consideration: Juries may now be encouraged to take into account the natural flow of events and additional corroborating evidence when determining causation.
- Refined Legal Standards: Legal practitioners and courts alike may begin to revise the rigid definitions of what constitutes “clear and convincing” evidence, potentially leading to a more nuanced approach.
- Increased Plaintiff Confidence: Plaintiffs could become more confident that their case will not be summarily dismissed on the basis of expert testimony that merely qualifies negligence as “likely.”
- Enhanced Accountability: Medical practitioners and institutions might feel added pressure to ensure that all relevant tests and procedures are thoroughly completed, knowing that failures in protocol could be more effectively scrutinized under this broader evidential framework.
These outcomes, while promising for those seeking justice, also introduce a degree of uncertainty and complexity for healthcare providers who now face the possibility of more detailed evaluations of their emergency procedures.
Expert Evidence and Jury Deliberations: A Closer Look at How Juries Might Weigh “Likely” Testimony
In making its decision, the court noted that it was not asserting that a plaintiff’s expert testimony alone could satisfy the evidence requirement. Instead, it emphasized that such testimony should trigger a more comprehensive inquiry into the complete body of evidence available in the case. This decision acknowledges that while the phrase “likely” is not synonymous with the definitive proof required by the “clear and convincing” standard, it nonetheless provides a valuable insight into the causation issue.
Juries, when tasked with evaluating these cases, are essentially being asked to put together a puzzle with pieces that may at first seem incomplete or vague. The court’s language suggests that juries are expected not only to assess the expert testimony in isolation but also to consider the entire narrative that the evidence tells. This might involve:
- Cross-Examination and Credibility Assessments: Juries will have the opportunity to assess the credibility of experts whose opinions express uncertainty through the term “likely.”
- Weighing Multiple Sources: The role of the jury becomes critically important in synthesizing disparate types of evidence—from medical records to witness accounts—to determine if the standard of “clear and convincing” evidence has ultimately been met.
- Understanding the Chain of Events: A detailed examination of the timeline and sequence of events may allow juries to find that, despite some ambiguity in expert language, the overall evidence creates a coherent narrative of cause and effect.
This more inclusive approach could help bridge the gap between the often abstract language used by medical experts and the concrete facts that juries are better equipped to evaluate when considering the outcome of a malpractice case.
Impact on Healthcare Providers: Managing Your Way Through the Complicated Pieces of Legal Risk
Healthcare providers now find themselves in a position where legal risk in emergency settings must be managed with an awareness of these evolving legal standards. While the decision does not relax the expectations for medical care, it does mean that hospitals and emergency departments may soon face increased scrutiny regarding their treatment processes. There are several critical ways in which healthcare institutions might need to adjust:
- Improved Documentation: To support their defense in potential malpractice suits, providers may need to enhance the documentation of patient care, especially in cases where initial tests and diagnostic steps are pivotal.
- Enhanced Training: Medical staff might receive additional training on the importance of following through on urgent care recommendations and documenting each step of the process with precision.
- Protocol Revisions: Hospitals could consider revising emergency room protocols to ensure that any indications of severe infections or complications, such as bacterial endocarditis, are thoroughly investigated.
- Risk Management Communication: Clear internal communication strategies can help ensure that all staff members are aware of the legal implications of inadequate testing or poor documentation.
The decision by the Arizona Supreme Court, while intended to balance the scales of justice for plaintiffs, also serves as a reminder to healthcare providers of the need to meticulously manage the legal aspects of patient care. By being proactive about these changes, hospitals may reduce their vulnerability to malpractice claims and improve overall patient safety standards.
How Jury Deliberations Could Change: Taking the Wheel in Medical Malpractice Trials
The ruling implicitly reaffirms the importance of the jury’s role in interpreting not only expert testimony but the entire body of evidence presented during a trial. This shift encourages juries to take a more active part in sorting out the myriad small distinctions and fine shades of evidence that contribute to a case’s overall narrative.
This approach can be summarized by looking at the jury’s tasks during a malpractice trial:
| Jury Task | Description | Examples in Practice |
|---|---|---|
| Evaluating Expert Testimony | Assessing the credibility and reliability of expert opinions, including those using terms like “likely.” | Reviewing the methodology behind the expert’s conclusions on bacterial endocarditis causation. |
| Reviewing Medical Records | Analyzing detailed patient records to understand the sequence of events and treatments administered. | Comparing documentation from urgent care and emergency room visits. |
| Consideration of Supplementary Evidence | Incorporating additional proofs, such as witness statements, to build a comprehensive picture. | Testimonies from nurses or other medical staff involved in the care of the patient. |
| Synthesizing a Narrative | Piecing together all evidence to determine if the standard of “clear and convincing” evidence is met. | Creating a timeline that correlates doctor recommendations, tests administered, and treatment outcomes. |
This table underscores that the jury’s role is far from passive. Instead, it requires them to actively engage with the evidence and figure a path through the complicated pieces and subtle details that define each case. The decision suggests that juries are fully capable of working through these tricky parts, provided they have access to all relevant facts and a clear explanation of what the evidence implies.
Future Reforms and Legal Considerations: Digging Into the Hidden Complexities of Causation Proof
Looking ahead, legal analysts believe that the Arizona Supreme Court’s decision may prompt further reforms in the realm of medical malpractice litigation. Given the evolving nature of medical technology and evidence gathering, several potential areas for future reform have emerged:
- Refining the Evidentiary Standard: Future cases could see a more adaptive interpretation of what “clear and convincing” evidence entails, with an increased focus on the overall narrative rather than isolated expert opinions.
- Enhanced Training for Legal Professionals: Attorneys specializing in medical malpractice might benefit from additional training in understanding the fine points of medical evidence, including the subtle parts that often come into play during an emergency room scenario.
- Better Communication of Medical Procedures: Hospitals and legal teams alike may work towards clearer articulation of emergency protocols—not only for patient safety but also to ensure that the evidence is presented in a way that juries can easily follow and understand.
- Interdisciplinary Collaboration: Collaboration between the medical and legal communities could lead to the development of new guidelines for documenting and verifying medical procedures, thereby reducing the likelihood of negligence claims stemming from miscommunication or incomplete records.
Such reforms would be super important not only for maintaining high standards in medical care but also for ensuring that the legal system accurately reflects the realities of modern healthcare. With the increased reliance on technology in diagnosing and treating patients, the hidden complexities of causation proof are bound to evolve, requiring both legal and medical professionals to keep up with the latest methodologies and definitions.
Moreover, this approach may spill over into other areas of the law where similar challenges exist—situations where expert judgment is inherently intertwined with the natural sequence of events. The decision encourages legal practitioners to take a closer look at how evidence is weighed and to consider whether the binary approach of dismissing testimony as “likely” versus “clear and convincing” is adequate for modern legal challenges.
Practical Steps for Legal and Medical Professionals: Finding Your Path Through the New Evidence Paradigm
In light of this ruling, professionals from both the legal and medical fields must prepare for the changes that lie ahead. While the Arizona Supreme Court’s decision does not immediately change the definition of negligence or the standard of proof, it does influence how cases are initially approached and assessed in court. Here are some practical steps that could be taken:
-
Legal Professionals:
- Review current case law to understand how “likely” testimony has been treated in the past.
- Update trial strategies to include comprehensive evidence discussions that incorporate all facets of a patient’s experience.
- Engage with medical experts early on to ensure that testimony is constructed in a manner that supports a narrative of causation.
- Consider mock jury trials to better anticipate how a jury might interpret evidence presented in this new light.
-
Medical Professionals and Institutions:
- Enhance documentation practices to create an unbroken, detailed timeline of patient care.
- Implement rigorous internal audits to ensure diagnostic tests and treatments meet the highest standards.
- Facilitate training sessions on the legal implications of incomplete or ambiguous documentation.
- Collaborate with legal experts to understand emerging legal trends and adjust institutional policies accordingly.
These steps not only help mitigate legal risks but also promote a higher level of care. Improved communication between medical staff and legal advisors can lead to a better understanding of what is needed to satisfy the evidentiary requirements in malpractice lawsuits.
A Closer Look at the Jury’s Role: Taking Control in a Changing Legal Environment
The Arizona Supreme Court’s decision fundamentally reaffirms the jury’s power to interpret and synthesize evidence in a manner that goes beyond rigid definitions dictated by the wording of expert testimony. This approach embraces the reality that the process of establishing causation is rarely cut and dried, especially in emergency scenarios where medical decisions must be made quickly and under intense pressure.
By encouraging juries to consider a broader range of evidence, the court places trust in the collective wisdom of the jury. This not only democratizes the determination of causation but also emphasizes the jury’s duty to piece together the sequence of events, testing the limits of what might otherwise be seen as nerve-racking legal ambiguities.
The benefits of this method include:
- Holistic Evidence Review: Juries are no longer forced to rely solely on stringent expert language, but rather, they can look at all available evidence in totality.
- Improved Judicial Outcomes: Cases that might have been dismissed prematurely may now be given a fair hearing, potentially leading to more just outcomes.
- Greater Accountability: The decision fosters accountability among medical professionals by ensuring that each step in patient care is subject to close judicial examination.
This shift could also influence how future juries are instructed by trial judges, focusing on the need for careful deliberation over the varied evidence rather than a narrow reliance on a single piece of expert testimony.
Reflections on Balancing Justice: Weighing the Evidence in Life-and-Death Cases
In cases such as Henke v. Hospital Development of West Phoenix, Inc., the stakes could not be higher. A family is left grappling with loss while the legal system strives to determine whether negligence truly led to a preventable outcome. The challenges presented by the “likely” causation terminology reflect the broader difficulties of addressing real-life tragedies within a legal framework.
For many, the ruling is a step toward ensuring that every piece of evidence is given its due consideration, rather than dismissing a claim because it doesn’t neatly fit into a predetermined formula.
As we take a closer look at the evidence and work through these tricky parts of medical malpractice cases, it becomes clear that the path to justice is rarely straightforward. Instead, it is full of small distinctions, subtle details, and a need for a comprehensive examination of all available evidence.
The decision also prompts critical reflection on how legal standards are applied to complex scenarios. When the very methods used to determine causation are open to reconsideration, both healthcare providers and legal professionals must be ready to adapt their practices and expectations to better serve the cause of justice.
Future Outlook: Sorting Out the Tangles and Adjusting to a Broader Evidentiary Landscape
Looking forward, the implications of this decision could extend well beyond individual cases. Legal scholars and practitioners alike are now contemplating future reforms which may include:
- Revisiting Evidentiary Standards: Legislators and judges might need to reassess what constitutes “clear and convincing” evidence in the context of emergency care, taking into account the unpredictable nature of medical interventions.
- Enhanced Expert Collaboration: Closer relationships between legal professionals and medical experts could foster better communication and understanding, ensuring that expert testimony is both accurate and comprehensible to juries.
- Policy Adjustments: Hospitals and emergency care centers might implement new policies designed to minimize risks and improve the overall standard of care, thereby reducing the potential for malpractice claims.
- Interdisciplinary Training Programs: The development of training programs that bring together legal and medical professionals to discuss case studies and share best practices could help bridge the gap between the two fields.
Regardless of how the landscape evolves, this decision highlights the importance of rethinking traditional legal frameworks in light of modern evidence and the realities of emergency medicine. It invites all parties involved to take a closer look at every step of the patient care process and to make necessary adjustments that ensure justice is served without compromising the quality of medical treatment.
Final Thoughts: Embracing a More Comprehensive Evidence Process in Medical Malpractice Litigation
The Arizona Supreme Court’s ruling is a call for a more nuanced and holistic approach in evaluating malpractice cases, particularly those originating in the high-stress environment of emergency rooms. By allowing expert testimony that qualifies negligence as “likely” to remain under consideration, the court empowers juries to piece together the full narrative of a case—one that reflects the natural sequence of events rather than a simplified, binary standard.
This approach may ultimately lead to more equitable outcomes for families who have suffered from medical oversights, while also pushing the medical community to reexamine their protocols and documentation practices.
In a legal arena often loaded with problems and tension, this decision serves as a reminder that the pursuit of justice is an evolving process—one where every fine point matters and where the jury is trusted to work through the complicated pieces of evidence to reach a fair verdict.
As practitioners from both law and medicine take their place in this shifting landscape, it is essential that they remain open to change, meticulous in documenting each step of patient care, and willing to collaborate for the greater good. After all, in cases where lives hang in the balance, every subtle detail and every slight difference in evidence can make all the difference.
By embracing a more comprehensive evidentiary process, both legal professionals and healthcare providers can help ensure that the outcomes of future medical malpractice cases reflect not only the letter of the law but also the inherent complexities and unpredictable twists and turns that define human life and medical care.
This ruling is not just a legal adjustment; it is a call to reexamine how we define and approach negligence in an era where quick decisions can have life-or-death consequences. It challenges us to look beyond rigid categories and to piece together a fuller picture—one that accurately captures the ripple effects of each moment of care, and one that ultimately supports the goal of equitable and just outcomes.
In conclusion, the Arizona Supreme Court’s decision on the admissibility of expert testimony that notes negligence as “likely” is set to have far-reaching impacts on the conduct of medical malpractice litigation. Whether viewed as a win for plaintiffs seeking justice or as an invitation for improved standards in medical documentation and care, this decision reminds us all that the path to justice is often full of tangled issues and nerve-racking challenges—challenges that must be met with careful deliberation, a commitment to thorough evidence review, and a willingness to consider every little twist that life throws our way.
As the legal community reflects on this precedent, it is essential to remember that while the journey through emergency room malpractice cases may be filled with confusing bits and intimidating obstacles, the ultimate goal remains clear: to ensure that every patient receives the quality care they deserve—and that every voice is heard when seeking accountability in the midst of tragedy.
Originally Post From https://www.azfamily.com/2025/10/23/arizona-supreme-court-clarifies-standard-medical-malpractice-cases/
Read more about this topic at
Arizona Supreme Court clarifies standard for medical ...
What the Standard of Care Means in Medical Malpractice ...








No comments:
Post a Comment