Examining the Shift in CDC Immunization Policy
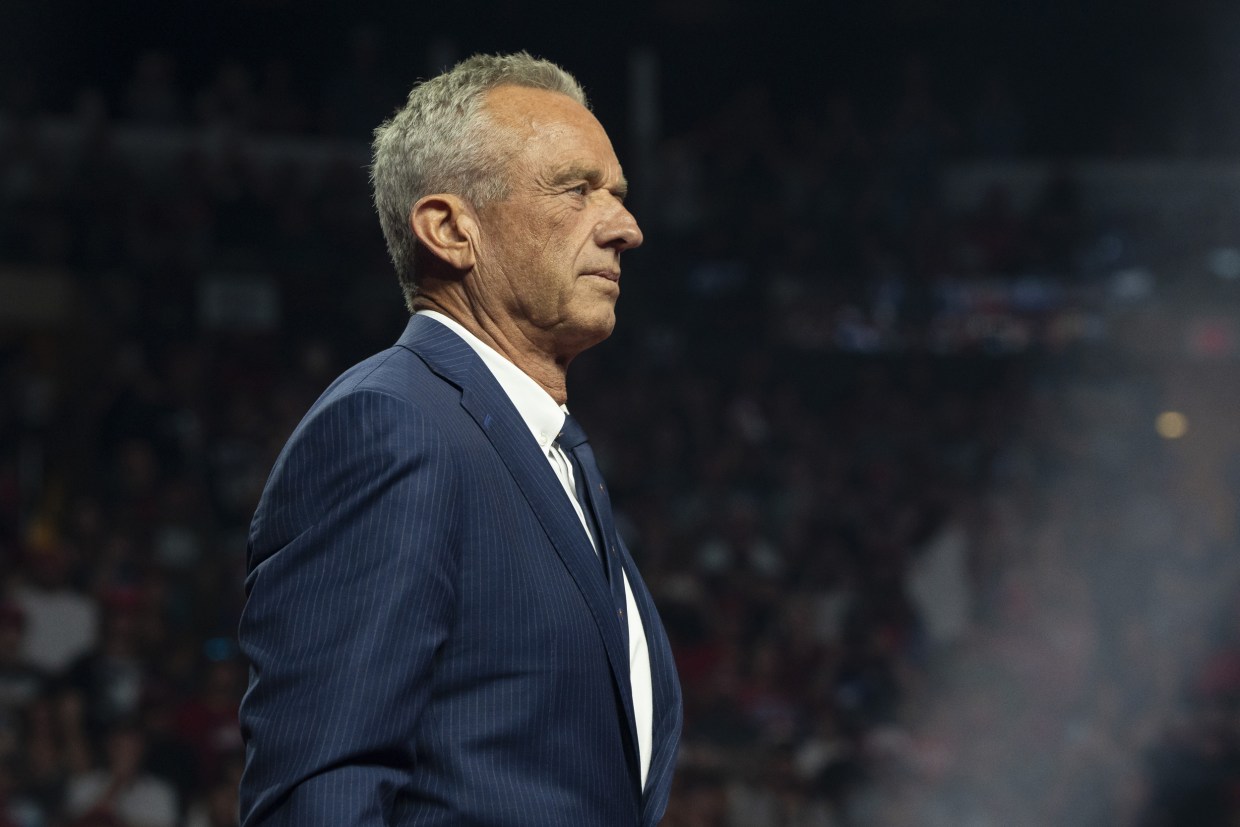
The recent decision by HHS Secretary Robert F. Kennedy Jr. to remove the Covid-19 vaccine from the CDC’s recommended immunization list for healthy children and pregnant women has sparked a heated debate among legal experts, public health advocates, and industry stakeholders. This move, delivered over a short video announcement on a prominent social media platform, raises a number of legal questions, as well as concerns regarding due process and transparency in government policy-making.
The announcement not only marks a significant shift in public health policy but also illuminates a range of tricky parts in administrative procedure practices. With key CDC officials notably absent from the announcement—and with little insight into the research or public feedback that may have informed the decision—many are left questioning the fine points of this policy change.
Understanding the Administrative Procedures and Legal Precedents
One of the first areas that warrants close attention is the administrative procedure that underpins major policy changes in government agencies. By removing the Covid-19 vaccine from the list without a clear, public explanation or documented feedback process, the decision risks being viewed as a departure from standard regulatory practices.
Legal experts argue that when an official pronouncement diverges from established guidelines, there must be a careful and methodical process in place. In theory, any changes to a vaccine recommendation should include:
- A comprehensive analysis of the available scientific data
- A notice and comment process to gather public input
- Clear documentation of how studies and statistics influenced the final decision
This approach is intended to help all interested parties—ranging from doctors to patient advocacy groups and even state regulators—understand the rationale behind such decisions.
Without this clear documentation, questions arise not only regarding the legal authority behind the decision but also about whether established statutory requirements were followed. Experts like Brian Dean Abramson have stressed how any change to existing policy should be done with a transparent process that includes public commentary. The current situation, however, leaves many to ponder if the procedures have been properly observed, given the absence of detailed evidentiary support and the lack of engagement with the CDC's Advisory Committee on Immunization Practices.
Potential Legal Challenges and Public Health Implications
The legal community is now watching closely as this decision could trigger multiple lawsuits, especially on procedural grounds. Several key issues stand out:
- Procedural Flaws: The decision appears to have been made without the standard notice-and-comment process. This omission could provide a basis for legal challenges centered on administrative fairness.
- Scientific Justification: With little clarification offered regarding the scientific research or public health data supporting the decision, critics argue that the move might be seen as arbitrary, potentially undermining trust in the CDC’s processes.
- Impact on Vaccine Coverage: Removing the vaccine from the recommended list may influence how health insurers cover the immunization. If insurers decide to drop coverage or impose cost-sharing, the consequences could be significant for accessibility, especially for populations already vulnerable to severe outcomes from Covid-19.
In this context, the legal challenges may not solely be rooted in the procedural missteps. Instead, they could also address the broader implications of the policy for groups such as physicians, patients, and even vaccine manufacturers who may have expectations based on previous government endorsements.
Law professors, including those from prestigious institutions, have suggested that if a challenge to this decision is successful, it may rest on the argument that the necessary procedural guardrails were not followed. This could set important legal precedents, influencing how future policy changes are managed regarding vaccine recommendations.
Questions Surrounding Public Input and Transparency
A significant aspect of the debate centers on the role of public input in shaping health policy. Many feel that a decision of this magnitude should be the result of extensive public debate and discussion. Without an open forum, affected parties—ranging from healthcare providers to the general public—may be left in the dark about the reasons for the change and what evidence was considered.
Public transparency is key not only to a healthy democratic process but also to ensuring that policy decisions are made based on a broad spectrum of considerations. In the present case, critics point out that:
- The absence of CDC representation: The fact that no CDC official was part of the initial announcement means that those who rely on the agency for guidance are left wondering about the insider details of the decision-making process.
- Lack of stakeholder commentary: There is no clear indication that an opportunity for public comment, particularly from healthcare professionals and vaccine manufacturers, was given prior to the announcement.
- Scientific documentation: The decision did not outline which studies or data were used to justify the removal of the vaccine recommendation—leaving many to question the scientific rigor behind the choice.
The expectation is that any change bearing significant public health implications should be accompanied by a thorough explanation, detailing the small distinctions between past recommendations and the current stance. Such transparency not only helps to build trust with the public but also safeguards the administration from potential litigation down the line.
Impact on Healthcare Providers and Insurance Coverage
The decision to withdraw the Covid-19 vaccine from the CDC’s list of recommended immunizations may have a ripple effect in the healthcare sector. For many healthcare providers, following the CDC’s guidance is a critical part of their daily operations. If the guidance shifts without clear evidence or proper notification, it creates a set of translated challenges that need to be addressed:
- Medical Uncertainty: Physicians are left figuring a path through conflicting information. Without updated guidance supported by robust research, determining the best course of action becomes a nerve-racking task.
- Insurance Implications: Many health plans base their coverage on CDC recommendations. Should insurers drop coverage or introduce cost-sharing for the Covid-19 vaccine, patient access may become severely restricted. The potential financial burden on patients could widen the gap in healthcare equity.
- Legal Liability: Physicians and hospitals might find themselves facing legal questions if patients or advocacy groups claim that changing immunization guidance led to harm. Without a well-documented rationale, defending against such claims could become off-putting and complicated.
This area is particularly loaded with issues, as the interplay between public policy, legal mandates, and healthcare administration creates many tangled issues. The reduction in vaccine coverage could ultimately lead to a decrease in vaccination rates among younger populations and expectant mothers, potentially impacting community health outcomes.
In addition, many in the industry are concerned that mixed signals may foster confusion among the general populace during an already challenging time. If public trust in the CDC declines, the social contract between the government and its citizens becomes increasingly strained.
Industry Concerns: Vaccine Manufacturers and Regulatory Takings
The fallout from this decision extends beyond public health and administrative law—it may also have significant financial and regulatory effects on vaccine manufacturers. Companies like Pfizer, Moderna, and Novavax find themselves in a precarious position where regulatory decisions can affect both their market value and their future investments in vaccine research and development.
Experts in regulatory law have recognized that vaccine manufacturers could perceive this decision as a government action that effectively limits their ability to distribute a product on which they heavily relied. Among the key concerns raised are:
- Statutory Requirements for Narrowing Indications: Manufacturers may legally question whether the government adhered to the statutory requirements when narrowing the indication for vaccine usage, especially without new data to support the change.
- Regulatory Taking Claims: There is the possibility that vaccine makers might claim a regulatory taking—arguing that the decision effectively confiscates their product rights without appropriate compensation. This could set off a series of lawsuits against the government, further intensifying the legal debate.
- Market Implications: The reduced usage of Covid-19 vaccines among certain demographic groups might affect future production and research funding. Manufacturers must now consider not only the immediate financial loss but also the long-term impact on product development and innovation.
Industry observers have noted that the decision roster seems unusual in that FDA Commissioner Marty Makary and NIH Director Jay Bhattacharya were mentioned in the announcement, even though their agencies are not responsible for vaccine recommendations. Instead, their roles traditionally involve vaccine licensing and research support, respectively. This misalignment raises further questions about the internal communication across federal agencies and the potential for conflicting directives in future public health policies.
A table summarizing some of the main concerns for vaccine manufacturers is presented below:
| Concern | Description |
|---|---|
| Procedural Oversight | Failure to follow standardized notice and comment process before making significant policy changes. |
| Regulatory Taking Claims | Potential for companies to argue that the government is impinging on their rights without proper compensation. |
| Market Access | Alterations in vaccine recommendations could lead to decreased market demand and altered supply contracts, affecting revenue streams. |
| Data Transparency | Lack of clear evidence or scientific backing for the recommendation shift, possibly leading to legal disputes. |
As these concerns percolate, it becomes clear that the decision is not merely a shift in public health policy but a move that could reshape the legal and regulatory landscape for vaccine distribution and public health management in the coming years.
The Role of Public Health Institutions in Policy-Making
One of the core issues in this debate is the evolving role of public health institutions like the CDC in shaping and implementing vaccine policies. Traditionally, the CDC has been the gold standard for immunization guidelines, relying on a review process that highlights extensive research, diverse stakeholder engagement, and a firm commitment to public health. However, the recent changes have exposed some confusing bits regarding who is steering this process.
Concerns have been raised by industry observers regarding the apparent absence of CDC officials in the decision process. Instead, influential figures from other institutions have taken center stage without clear accountability for the decision. This shift poses a challenge for the public in understanding and trusting the source of the guidance.
The following bullet list outlines some of the potential consequences of these changes:
- Institutional Trust: If the trusted CDC is seen as disconnected from key policy decisions, public confidence in federal health recommendations may wane.
- Decision Making Transparency: A lack of clear documentation and public dialogue can lead to speculation and uncertainty regarding the intent behind policy moves.
- Internal Coordination: When multiple federal agencies appear to be involved without clear roles, it creates an environment loaded with tension and signals a need for better inter-agency communication protocols.
In such a tense environment, it is essential that all agencies work together more cohesively to ensure that the public is neither misinformed nor left anxious about basic healthcare advice. Increasing transparency and engaging in public discourse about the decision-making process could help in restoring faith in science-based policymaking.
Legal Theories: Procedural Missteps and the Rule of Law
This case also warrants a closer look at the legal theories that could ultimately shape the outcome in courts. Several aspects of the decision may be ripe for exploration in a judicial setting, particularly those relating to procedural missteps and whether the change adhered to the rule of law. The decision might be challenged on several fronts:
- Due Process Violations: Critics argue that bypassing the standard notice and comment process deprives affected parties of an opportunity to participate in the policy-making debate.
- Lack of Factual Basis: The decision appears to be made with little documentation of the supporting scientific research, which could constitute a violation of statutory guidelines that require a factual basis for safety recommendations.
- Equitable Concerns: For groups that rely on full vaccine coverage—such as children and pregnant women—the removal from the recommended list could lead to inequitable access to healthcare, potentially triggering claims on grounds of discrimination or unfair treatment.
Legal experts emphasize that ensuring the integrity of governmental decisions is a key responsibility of the judiciary. In this case, courts may be called upon to sort out whether the administration followed the necessary procedures when making this substantial policy reversal. If found wanting, the decision might be reversed or forced to go through a properly documented review process.
Ultimately, the resolution of these legal questions will rely on a careful evaluation of the small distinctions—the fine points—that separate an administratively sound decision from one that offloads responsibility onto vulnerable populations without adherence to established laws.
Broader Implications for Public Health Governance
This policy shift is emblematic of wider trends in public health governance, where administrative decisions carry both far-reaching public health implications and significant legal consequences. As government agencies continue to refine their approach to managing the Covid-19 pandemic and other health crises, the process by which decisions are made becomes more critical than ever before.
Key areas that require closer consideration include:
- Accountability Mechanisms: The need for clearly defined roles and responsibilities among federal agencies is more pressing than ever. Ensuring that agencies like the CDC are at the forefront of their areas of expertise is essential for public trust.
- Feedback Integration: A robust public input process should be integral to any decision that bears widespread impact. By genuinely incorporating feedback from stakeholders and the public, administrations can not only protect themselves legally but can also foster greater societal cohesion during challenging times.
- Consistency in Policy-Making: Maintaining a consistent approach to updating health guidelines is a must-have in public health management. Sudden or poorly explained shifts in policy leave room for misinterpretation and possible legal fallout.
A diagram outlining the decision-making process might help clarify these areas:
| Stage | Description |
|---|---|
| Data Collection | Gathering current scientific research and public health data. |
| Public Consultation | Engaging stakeholders through notice and comment to incorporate diverse viewpoints. |
| Review and Analysis | Analyzing the data against existing guidelines and statutory requirements. |
| Policy Formulation | Drafting new recommendations and establishing a clear rationale with supporting documentation. |
| Announcement | Publishing the decision with transparency regarding both the process and evidence used. |
This structured approach underscores why it is critical that the current decision be revisited in terms of its procedural soundness, especially given its wide-reaching effect on public health practices and legal norms.
Assessing the Long-Term Impact on Legal and Regulatory Frameworks
Looking further ahead, the current dispute may have a lasting influence on how legal and regulatory frameworks are interpreted and applied in public health policy. If courts decide that the decision was improperly made, it could lead to more stringent requirements for regulatory agencies to document and justify their policy changes in the future.
Several long-term issues are on the horizon, including:
- Setting Legal Precedents: A courtroom ruling could define how much flexibility federal agencies have in altering vaccine recommendations without a lengthy public process.
- Revisiting Regulatory Standards: There may be calls for reform to ensure that all significant public health decisions are buttressed by robust, documented evidence and open public dialogue.
- Public Confidence: The manner in which regulatory agencies manage this transition could either bolster or diminish public trust in federal health recommendations for years to come.
Finding your way through these challenges will require that both legal and regulatory bodies take a hard look at the current methodologies. While ensuring compliance with existing statutory mandates is critical, fostering an environment where the public and all stakeholders remain informed and engaged is equally important for sustaining trust in government decisions.
Charting the Future Course for Public Health Policy
In conclusion, the decision to remove the Covid-19 vaccine from the CDC’s recommended immunization list poses a series of legal, regulatory, and public health challenges that are intertwined and full of problems. There is no simple path forward, but it is clear that enhanced transparency, better internal coordination among agencies, and more inclusive public dialogue are essential steps to avoid missteps in the future.
The legal community, healthcare providers, and industry stakeholders are now left to debate the proper balance between administrative flexibility and the need for procedural safeguards. The potential lawsuits and regulatory reviews that may follow this decision serve as a reminder of the importance of following well-established procedures—especially when the outcomes affect vast segments of the population.
As federal agencies continue to update their policies in response to evolving scientific knowledge and public health needs, this case serves as a cautionary tale. It underscores the risks that emerge when decisions are made without engaging all necessary stakeholders or providing clear, documented justifications. Looking ahead, it is super important that policy makers build in processes that are both thorough and collaborative, so that future health recommendations are not only legally sound but also command the trust of the public.
Final Thoughts: Balancing Decision-Making and Stakeholder Trust
Ultimately, navigating this new terrain in public health governance demands that all parties—government, legal experts, healthcare professionals, and industry representatives—take a close look at the underlying issues that have surfaced. The change in the CDC’s immunization list, though intended to reflect current scientific and medical perspectives, must be backed by a process that is as transparent as it is rigorous.
The decision’s hidden complexities, from procedural omissions to gaps in public communication, highlight the need for a reevaluation of how pivotal policy changes are implemented. Whether this move will lead to improved practices or further legal disputes remains to be seen, but one thing is certain: the stakes are high, and every stakeholder must work together to find a path that safeguards public health while respecting established legal frameworks.
In the coming months, as debates continue and potential legal challenges are mounted, all eyes will be on how federal agencies adjust their processes. The outcome will likely shape not only the future of Covid-19 vaccination policies but also the broader landscape of public health administration. Now is the time for decision makers to figure a path that not only addresses immediate concerns but also builds a foundation of trust, accountability, and scientific integrity for the future.
It remains to be seen how the intricate interplay between legal oversight, public policy, and government transparency will evolve in response to these developments. For now, the dialogue is ongoing, and the court of public opinion—as well as the actual judicial courts—will ultimately be the arena where these complex, nerve-racking issues are sorted out in the months and years to come.
Originally Post From https://news.bloomberglaw.com/health-law-and-business/court-challenges-loom-as-rfk-jr-cuts-covid-shot-from-cdc-list
Read more about this topic at
The CDC is no longer recommending Covid vaccines for ...
Controversy on fair and exclusive vaccine decisions for ...








No comments:
Post a Comment